Relationship-Building Strategies for Adoptive and Foster Parents to Address Picky Eating and Feeding Challenges
Adoption Advocate No. 123
Feeding and mealtimes are rich with opportunities for families to build trust and attachment, but when things aren’t going well, those opportunities are lost. From hoarding to picky eating, worries and battles around food and nutrition are common challenges adoptive and foster families face. About half of all preschool-aged children in America are described as “picky” by parents, roughly 10 percent experience more “extreme” and persistent picky eating, and up to 80 percent of children with special needs struggle similarly.
“Extreme picky eating is when a child or adolescent eats so little variety or amount of food that it impacts their physical, social or emotional development, or causes significant conflict or worry for the family.”
— Rowell and McGlothlin in Helping Your Child with Extreme Picky Eating
This article will introduce why adopted and foster children may be reluctant to eat; this understanding provides the framework for professionals to support parents with best-practice responsive feeding strategies that bring peace to mealtimes and help children eat and grow to the best of their abilities.
Consider this scenario: I was observing a family with children by adoption at lunch. Mom and Dad were attentive, loving, affectionate, and working really hard to get the kids to eat. Mom counted and announced every bite to Dad. Mom repeatedly put food into the children’s mouths or up to their mouths, encouraging and imploring them to eat, “Just one bite, it’s the cheese, that’s the best part!” The children turned their heads, clamped their mouths shut, and pushed Mom away. At one point, Mom playfully tried reverse psychology, “Oh, no! Don’t you dare take a bite of my sandwich, no eating MY sandwich!” Everyone was frustrated, no one was having a good time, and the children weren’t eating. These parents were doing their best, and falling into common feeding traps.
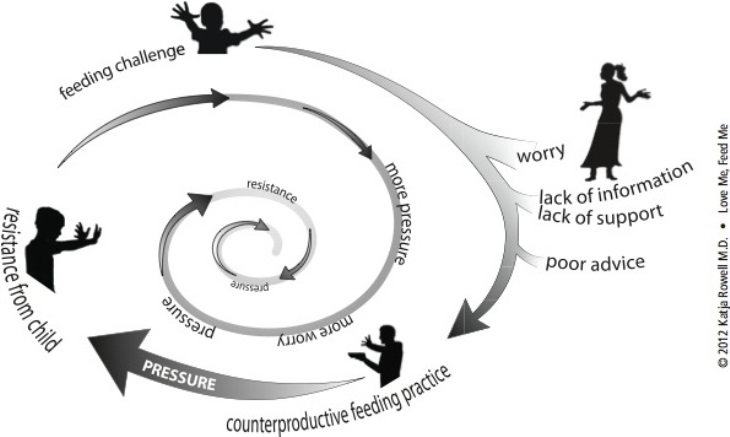
Most of the clients I have worked with felt stuck trying to get children to eat for months or years. This “Worry Cycle” explores the dynamic:
Why Might a Child Struggle to Eat?
It is not enough to see the ‘behavior’ of a child refusing to eat and then try to make them eat. We must understand why a child is reluctant. Essentially, anything that makes eating, swallowing, or digesting difficult, uncomfortable, or painful can lead to a reluctance to eat. Reflux, chronic constipation, neuromuscular or anatomic abnormalities of the airway or swallowing tubes, frequent infections, stressful procedures or surgeries, and certain medical and congenital conditions can make eating more challenging.
Unsupportive early feeding, including not being fed enough, fed while lying flat, served a limited variety, or offered only liquids or purees long after the time when table foods should have been introduced make sensory and oral-motor problems more likely. Traumatic experiences such as choking or forced feeding are aversive and may lead to an understandable avoidance of eating.
Sensory-motor integration challenges can make eating uncomfortable and difficult—even scary—if a child can’t chew and swallow predictably and safely. Sensory challenges are more common in former preemies, children who experienced malnutrition in utero and after, children on the autism spectrum, and children exposed to substances in utero or who were neglected or abused. Toxic stress and anxiety can lead to low appetite and a strong preference for familiar foods.
Simply put, if early experiences have been unpleasant or difficult, children may mistrust eating and those doing the feeding. Building trust takes time.
Why Might a Foster or Adoptive Parent Struggle to Feed Well?
Feeding challenges may be met by overwhelmed, under-supported, and worried foster and adoptive parents. As one mother of adopted school-aged siblings shared,
“Despite having read a TON in preparation, I wish I had known how much feeding is a key for attachment, even for older children. I wish I had had more information that there was a good chance that the table could be a very difficult place for a while, and some of the reasons for that—that is, the possibilities of chewing/swallowing/sensory issues. I may have been better able to stay calm and let some things slide if my expectations of a happy family meal had not been met with such a slap in the face.”
Parents may also receive poor advice, even from doctors and feeding therapists such as, “Just make them eat,” “No child will starve himself,” “Do whatever you have to do to get food in,” and, “Withhold eye contact until he eats.” Such advice can lead to tremendous battles—and desperate parents. As a physician, I can sadly say that many of my colleagues receive little-to-no training in feeding and have been the source of harmful advice. Combine the lack of support with a primal need to nourish and perhaps pressure to make up for poor past nutrition, and parents understandably fall into maladaptive feeding tactics.
For example, two-and-a-half-year-old Amari’s mom brought Amari to her pediatrician, a speech therapist, and dietitian who were unable to offer meaningful support. A psychology appointment was almost two months away. Amari’s mom was terrified that Amari would need a feeding tube after gaining only nine ounces the previous year and with recent setbacks. “I would just sit there and scream at her to eat. I knew it was wrong.” (Amari’s story ends happily after parent education and support. They even canceled the psychologist appointment as things were going so well.)
What Are Counterproductive Feeding Practices?
Parents who worry a child isn’t eating enough or isn’t eating the “right” foods may try pretty much anything to get a child to eat—from sticker charts to rewards, begging, threats, and even physical force. Children naturally resist, some more than others, so the parent tries harder or different tactics, which are often met with more dramatic resistance. Research and clinical practice shows that the harder parents work to get food into a child, the less likely he is to eat and the more likely he is to grow less well. If a child is flooded with stress hormones at anxiety and conflict-filled mealtimes, they have a hard time tuning in to cues of hunger and fullness coming from their bodies, and are more likely to reach for familiar foods. This dynamic undermines the child’s appetite, worsens their eating, and is a barrier to trust and attachment.
To be clear, this is not to blame care providers. Caregivers seeking to nourish a reluctant eater often put in incredible effort and may feel desperate out of their love for their child. Health care providers and professionals need better training and education to support families.
Why Do Children Resist Pressure to Eat?
Each child is unique, but there are common themes. As Keck and Kupecky noted in Parenting the Hurt Child, hurt children often seek conflict—it’s familiar and feels safe. What better opportunity to pick a fight than mealtimes where the parents’ goals provide traction for pushing back? Ashley Rhodes-Courter’s book Three Little Words details her food-insecure early years and subsequent food battles with her adoptive mother, Gay:
“I knew Gay was trying to please me, but for some reason, I resisted every attempt she made. She made chicken nuggets in the oven so they’d have the KFC flavor but not as much fat. They were quite good, although I was annoyed by the way she preached to me about eating healthy foods.”
Children, in all kinds of situations, resist attempts to get them to eat to preserve autonomy, to test boundaries, to try to get their favorite foods, when they’ve had negative experiences and are protecting themselves, and when they don’t want to “lose” and eat a veggie. Even with a secure attachment, it is developmentally appropriate for many children to resist pressure as they seek independence. (Think the “terrible twos” or the resistant teen.) Pressure to eat is not helpful.
And of course, some children simply can’t eat, or need more facilitation. Children with oral-motor delays or sensory difficulties, children who have trouble swallowing safely, etc. will benefit from specialized support.*
Breaking the Cycle
Many parents feel that their only option is fighting over every bite of “healthy” food or only serving the child’s handful of carb-heavy favorites. There is another option, called responsive feeding, where the whole family can enjoy mealtimes, each other, and promote a healthier relationship with food. Putting effort into pleasant mealtimes and supportive feeding practices, rather than into battles over bites, will help children do better with eating. It is a win-win.
Responsive feeding can be used with children who are larger or smaller than average, picky or hoarding, with or without special needs, and who join a family by birth, foster care, or adoption. It is a relief for parents to feed all children at the table essentially the same way. It is a philosophy grounded in providing and nurturing within a structured and loving routine.
Here are some basics to share with parents and care providers:
Put best nutrition on the back burner for now. When it comes to nutrition, aiming for perfect is often the enemy of the good. Battling over foods now is likely to make a child’s long-term eating and nutrition worse. Allowing children to enjoy preferred and familiar foods, and try new foods (even if they are not nutritionally “ideal”) helps get families on track for the long-term goal of raising a competent eater. For example, fruit packed with syrup offers vitamins and fiber and can bridge to other fruits. Ketchup and other sauces are shown to increase the variety of accepted foods.
Professionals should support families before and early into placement. Anticipate potential challenges, inform, empower, and support parents with best feeding practices. Offer information and resources.
Parents’ worries need to be heard and addressed. A health care provider should conduct a thorough history and physical exam with laboratory analyses as appropriate. Red flags for oral-motor, sensory, or medical concerns require follow-up.
Reduce conflict and anxiety. Hunger and fullness signals are drowned out in a dysregulated body. As Ashley Rhodes-Courter shared, “As the adoption made me feel secure, the tautness in my stomach relaxed, and I found that I was interested in new foods. I realized that I could find something I liked at almost any restaurant, whereas before I had often left hungry.”
Attend to a child’s “heart” needs first. As Charlie Slaughter, MPH, RD, wrote in Hungry for Love, four things are fed by parents at mealtimes: “love, care, connection, and food.”
Serve at least one familiar and accepted food with every meal and snack (alongside foods the family eats and nutrient-dense foods without fuss) even if in the beginning familiar foods are mostly processed, crackers, or plain pasta.
Serve meals and snacks at predictable intervals. Care providers may want to offer food more often at first, even every hour or so. Assume the child has experienced food insecurity. Then space out meal and snack times to every two to four hours with mostly water in between. This helps children feel secure, completes attachment cycles, and supports appetite self-regulation.
Serve family- or buffet-style and help children serve themselves as needed. This is the #1 tip parents say diffuses mealtime battles. If parents pre-plate, the negotiating, whining, and anxiety can start before the plate even hits the table. Neutralize every battle possible.
Let manners go (for now) unless it interferes with social connection at the table. For example, let them eat with their fingers, but not hit a sibling.
Avoid talking about how much or what children eat. Don’t call them “picky.” Either children don’t want to disappoint adults and they feel badly, or they won’t or can’t comply. Either way, pressure to eat can turn kids off food, or teach them to overeat over time.
Reassure with simple phrases such as, “There will always be enough,” or “You don’t have to eat anything you don’t want to.”
Send the message that they can be trusted with their eating! Care providers can do this by putting the foods out, and then being good company and letting children do their jobs with eating. This is known as the Division of Responsibility. Children are in charge of how much they eat at meal and snack times.
Feed each child at their skill level. Prepare foods appropriate to varying skill levels. For example, start with serving sloppy joes or slow-cooked pulled chicken vs. starting with a tougher steak. A 3-year-old who has had little exposure to variety in flavor or texture may need foods prepared that are more typical for a young toddler. Consider an evaluation with an experienced speech pathologist to help parents know how best to support eating if a child seems to have trouble.* Most children, even with some oral-motor delays, don’t need therapy if they are meeting basic nutrition needs and are progressing.
Participate in food-related activities with no expectation that children eat. Pick berries, grow a basil plant on a window sill, paint with pudding, or make muffins for the teacher conference at school. Involving children in shopping or cooking in fun and rewarding ways is a great way to connect, engage the senses, and become familiar with new foods.
Allow opportunities to sample foods away from mealtimes. Explore samples at grocery stores such as Costco, Whole Foods, or Trader Joe’s. Buffets and parties where the focus isn’t on the food may be where a child feels safe to explore. I remember standing with a mom watching her little boy go back for four chicken satay sticks at a buffet. He ate happily with other children, enjoying the music and company. Mom shared that normally they bribe him to eat one or two bites.
Let children prepare and participate. Have children thread fruit on a wooden skewer, or allow them to spread hummus, peanut butter, or Nutella with a small dip spreader or knife. When children participate in food preparation, they are more likely (but not guaranteed) to eat. Remember not to nag.
Bridge to new foods through familiar foods. For example, put out plain noodles with possible sides like cheese, butter, or tomato sauce, or served cold with a mild dressing like a pasta salad. Serve with an accepted side.
Consider nutritional deficiencies. If a child accepts them, offer a chewable or other multivitamin, possibly iron, and a chewable DHA supplement.
Consult with the child’s doctor. These resources can help caregivers know when to consider testing and treatment.
Try not to predict what a child may or may not like. When taking a young family member out to a Middle Eastern restaurant, we thought she would like the warm, soft bread. Instead, she mostly ate the pickled vegetables. Try not to limit opportunities.
Serve a variety of foods, including fruits and veggies, many different ways. Take blueberries: Serve fresh, frozen (if children are old enough for it not to be a choking hazard), in pancakes, freeze-dried for crunch, in muffins, etc.
Support nutrition while building skills. Look for protein-enriched pastas, white whole wheat breads, whole grain Goldfish crackers, or calcium fortified juices. Try smoothies or milk shakes. Work with an RDN (registered dietitian nutritionist) if nutrition is truly limited.
Keep serving the foods the family enjoys and that children will learn to eat over time.
* Find the right help. If a child needs feeding therapies, be aware that there are different approaches. Therapies that ask a parent/care provider to withhold attention or affection to motivate a child to eat can harm attachment. Therapists should have some knowledge of trauma-informed practices and attachment. Here is a list of suggested questions and discussion points to help families find a therapy partner. If a child experiences increased anxiety, vomiting or gagging, or more conflict during therapies, a different approach may be advised.
Selective eating is rarely an emergency. Acknowledge that these changes can take time and help care providers brainstorm solutions to common obstacles such as a lack of time. It is not worth sacrificing connection and trust for short-term nutrition goals. These relationship-building feeding tips support children and families to come together at mealtimes, help children learn to eat based on signals of hunger and fullness, and head into adulthood with skills and habits that will support health and happiness for a lifetime.
References
- Helping Your Child with Extreme Picky Eating (Rowell and McGlothlin)
- Conquer Picky Eating for Teens and Adults (McGlothlin and Rowell)
- Mealtime Hostage blog and private Facebook support group
- Love Me, Feed Me: The Adoptive Parents’ Guide to Ending the Worry About Weight, Picky Eating, Power Struggles and More (Rowell)
- Healing From Food Insecurity: Beyond the Stash (Rowell)
- The Ellyn Satter Institute
- AdoptionNutrition.org by the SPOON Foundation
- Hungry for Love (Slaughter)
- A Practical Approach to Classifying and Managing Feeding Difficulties (Kerzner 2015). (Parents can share this with health care providers.)



